There are moments when policy data becomes personal. For millions of Americans, a change in how claims are reviewed can mean more secure benefits—or fewer hours of care. The Centers for Medicare & Medicaid Services covers over 160 million people and processes about 4.5 million claims per day. That scale shapes both promise and risk.
At the federal level, a deployed model achieved more than 90% precision, cut development from months to minutes, and flagged over $1 billion in suspect claims annually. Those are real operational benefits that protect program integrity and public funds.
Yet the Arkansas experience shows the other side: a 286-question algorithm that sorted beneficiaries into 23 fixed acuity groups led to widespread cuts in care hours. Implementation errors and incentive-driven design produced harm for people who rely on services every day.
We will explore both narratives—what improved within the system, and what went wrong—so leaders can act now to balance fraud prevention with humane outcomes.
Key Takeaways
- High-precision models can yield large operational benefits and expose suspect claims quickly.
- Design choices in an algorithm can reduce care and harm vulnerable people.
- Scale amplifies both savings and risks across federal programs.
- Transparent governance and human oversight matter for fair outcomes.
- Leaders must weigh program integrity against real-world effects on beneficiaries.
- Practical steps exist to protect benefits while maintaining system trust.
Executive summary: What this case study covers and why it matters today
Federal results and local failures sit side by side. Large federal deployments identified more than $1B in suspect claims annually with over 90% precision and cut model development time from months to minutes. Those figures show clear benefits for program integrity and efficiency.
The contrast is stark: a 2016 state tool reduced complex assessments to 23 fixed categories after 286 questions, and that translated into widespread cuts for people who depend on care. The UK Department for Work & Pensions’ fairness review found significant disparities by age, disability, marital status, and nationality—gaps some organizations still have not fully measured.
The central problem is balancing fraud prevention with access and due process. The path forward requires more than faster models: it demands fairness testing, explainability, and human review.
- Scope: How artificial intelligence and algorithms reshape benefits administration.
- Evidence: Scale and accuracy claims versus harmful local design choices.
- Way forward: Embed transparency, oversight, and clear avenues for appeal.
Understanding the landscape: Welfare fraud, error, and the promise of artificial intelligence
Understanding where fraud, error, and policy design overlap is essential for any agency that administers benefits. Stakeholders want clear answers: how detection works, who is affected, and what safeguards protect legitimate beneficiaries.
Informational intent: What people want to know about fraud and benefits
Officials, advocates, and recipients ask similar questions: which signals trigger review, how appeals work, and how errors are corrected. Clear thresholds and timely human review reduce wrongful cuts.
Scale and stakes: 160 million people and 4.5 million claims per day
CMS covers more than 160 million people and handles roughly 4.5 million claims per day. Even low false-positive rates can affect thousands of people quickly.
From waste reduction to human impact: Balancing efficiency with care
Estimates put fraud and improper payments at a meaningful slice of a $4T health care market. Faster patterns in data can shrink waste, but design choices—model thresholds, appeal paths, and oversight—determine whether savings harm access to benefits.
“Systems must protect program integrity without sacrificing the dignity and care of beneficiaries.”
| Dimension | Priority | Risk if Misapplied |
|---|---|---|
| Accuracy | High | Wrongful benefit cuts |
| Speed | Medium | Insufficient review |
| Transparency | High | Loss of trust |
| Human oversight | Critical | Bias amplification |
- Goal: Reduce waste while protecting benefits.
- Way forward: Pair models with clear governance and appeals.
Data, systems, and models: How algorithmic decision-making enters social benefit programs
Modern benefit systems feed on large streams of administrative records and operational logs. That flow shapes what is visible to analysts, vendors, and program staff.
What data is used and who has access
Claims histories, provider behaviors, beneficiary attributes, and program policy logs form the core data set. Each type carries different privacy obligations and retention rules.
Access governance matters: role-based controls and audit trails limit who can view sensitive information while supporting legitimate program work.
From rules to models: Algorithms and hybrid approaches
Systems vary: simple rules enforce policy thresholds, peer-reviewed statistical instruments provide transparent scoring, and machine learning models spot complex fraud patterns. Hybrid approaches often deliver the best signal by combining clarity with pattern recognition.
Information hygiene is essential. Data quality, lineage, and refresh cycles directly affect outputs and downstream decisions.
- Map: define sources, owners, and controls.
- Validate: peer-review models and preserve documented parameters.
- Govern: retain human override with logged rationale.
“Implementation discipline prevents validated instruments from becoming misapplied software.”
The Arkansas case: When an algorithm determines hours of care
A 2016 rollout in Arkansas turned a long nursing assessment into rigid categories that capped hours of support. The system used a 286-question instrument to place each person into one of 23 acuity groups. That group then determined fixed daily care allotments.
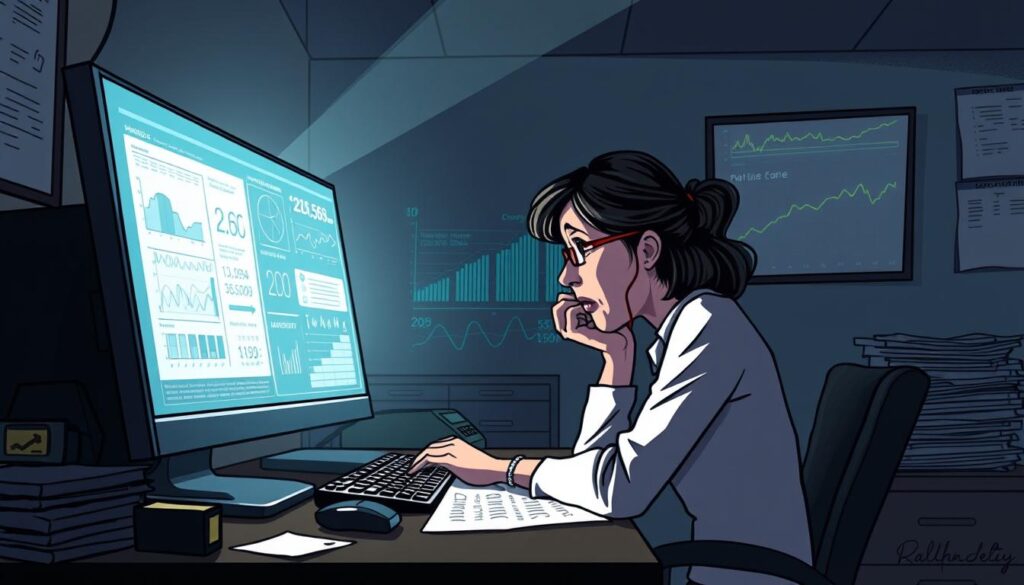
Assessment-to-decision pipeline
The pipeline reduced clinician judgment to categorical outputs. In practice, only a subset of items drove scoring; interaction effects formed opaque constellations beneficiaries could not decode.
Result: immediate reductions in benefits and fewer supports at home. Nurses reported, “it’s the computer”, not clinical discretion, that set hours.
Peer-reviewed research supported the underlying instrument, but the software implementation deviated and produced incorrect outputs.
- The design capped hours even when correctly configured, so many people lost care compared with prior years.
- Consequences included missed appointments, higher health risk, and family strain.
- The rollout prompted litigation and highlighted the need for validation, explainability, and fallback procedures.
For a detailed review of policy and system lessons, see our Arkansas implementation review at Arkansas implementation review. Rigorous testing, clear appeals, and communication plans are essential before any system changes affect real lives.
AI Use Case – Welfare-Fraud Detection: Performance metrics and operational wins
Operational wins emerge when agency teams, vendors, and data converge around clear goals. Federal deployments show that faster cycles and strong precision produce measurable program benefits.
Speed and scale: Cutting development from months to minutes
GDIT and CMS shortened model development time dramatically. What once took months now completes in minutes.
This faster time-to-production helps agencies respond to fast-moving fraud schemes each day.
Accuracy claims: Greater than 90% precision
Precision above 90% means flagged claims are well targeted. High precision reduces the burden on reviewers and lowers wrongful interventions.
Validation on out-of-sample data is essential to keep that precision stable over time.
Financial outcomes: More than $1B in suspect claims identified
At federal scale—160 million people and roughly 4.5 million claims per day—even small gains matter. Annual identification of over $1B in suspect claims shows material impact on stewardship of health care funds and benefits.
| Metric | Result | Operational effect |
|---|---|---|
| Precision | >90% | Fewer false flags; targeted review |
| Development time | Months → Minutes | Faster response to schemes |
| Annual flagged value | > $1B | Improved fund protection |
| Scale | 160 million people; 4.5M/day | Small gains magnify impact |
“Models must sit inside policy-aware systems with clear human review and feedback loops.”
Company-agency collaboration, domain expertise, and governance shape how algorithms preserve benefits while guarding the system against fraud.
Risks and real-world harms: Bias, wrongful cuts, and due process failures
Algorithmic reviews can reshape lives overnight when systems misalign with human judgment. Real-world examples show how quick automation can create lasting harm for people and beneficiaries.
UK analysis found statistically significant disparities by age, disability, marital status, and nationality. That evidence points to measurable bias in outcomes for individuals who sought advance payments.
In Arkansas, software deviations from an established instrument reduced care hours. Even properly configured, the design capped benefits and led to wrongful cuts.
Privacy risks rose where systems expanded collection without clear minimization, access controls, or disclosure. Michigan’s settlement after false flags shows the cascading harms a person faces: lost income, stigma, and legal costs.
“Due process requires clear notices, understandable reasons, and timely appeal paths for anyone affected.”
- Evidence: DWP fairness testing showed disparate impacts across groups.
- Human rights: care allocations and fraud suspicions must preserve dignity and recourse.
- Remedy: ongoing bias testing, published summaries, and prompt corrective actions.
| Risk | Evidence | Immediate effect |
|---|---|---|
| Bias | DWP fairness analysis | Unequal outcomes by group |
| Software error | Arkansas deviations | Reduced care hours |
| False flagging | Michigan settlement | Income loss, legal harm |
What worked in healthcare fraud detection: Lessons from CMS and enterprise AI
Operational teams learned quickly that data alone cannot replace subject-matter judgment. Federal engagements paired advanced analytics with clinicians and policy staff to tune practical solutions.
Pairing analytics with subject-matter expertise
Good models reflect policy reality. CMS projects show that features built with clinicians and auditors capture real-world signals. That alignment keeps outputs relevant to program goals.
Research-backed instruments, like peer-reviewed clinical tools, add methodological clarity. Implementation must match published specs to preserve validity.
Guardrails that matter: human-in-the-loop, validation, and monitoring
Human review is the primary safeguard. Tools should surface explainable outputs so reviewers can reason about each flagged case.
Validation protocols—pre-deployment testing, backtesting, and challenge datasets—confirm robust performance. Continuous monitoring detects drift in algorithms and shifts in fraud patterns.
| Practice | Why it matters | Operational effect |
|---|---|---|
| Domain collaboration | Aligns features with policy | Fewer false flags; better care outcomes |
| Explainable tools | Aids reviewer judgment | Faster, fairer decisions |
| Continuous monitoring | Detects drift | Maintains trust and system stability |
Global cautionary tales: Netherlands, Australia, UK—and lessons for U.S. social security
High-profile international missteps reveal how automated systems can upend public trust overnight.
The Netherlands wrongly accused about 20,000 families of child fraud. The government repaid roughly $32,000 per family and the cabinet resigned in 2021. That episode shows how a system error becomes a national crisis.
The Netherlands
Thousands of families faced wrongful scrutiny. The fallout included large repayments and political accountability.
Australia’s Robodebt
Robodebt accused roughly 400,000 welfare recipients. Courts found the program unlawful and the government repaid about $1.2B. The case highlights how flawed assumptions in automated tools produce financial harm.
UK DWP fairness analysis
The UK review found statistically significant disparities from automated vetting. Transparency gaps persisted on several protected characteristics, raising concerns about unequal outcomes for people and families.
“Systems deployed without testing and clear redress create widespread harms.”
- These examples expose a shared problem: weak governance, opaque algorithms, and limited recourse.
- Lesson for U.S. social security: mandate bias testing, publish impact reports, and require independent audits before scaling.
- Benefits administration must treat families and people as stakeholders—not just data points.
Governance and oversight: Building responsible fraud detection systems
“Define the problem precisely.” Fraud, error, and waste are distinct challenges. Each calls for a different level of intervention and a different operational response.
Define the problem: Fraud vs. error vs. waste—and proportional responses
Agencies should adopt a taxonomy that separates intentional fraud from clerical mistakes and program leakage. This prevents harsh measures that harm beneficiaries for administrative faults.
Calibrated responses mean targeted investigations for suspected fraud and simple fixes for errors.
Fairness testing and auditability: Documented variables, peer review, and red-teaming
Require documented variables and published research summaries. Peer review and red-team exercises expose blind spots and reduce disparate impact.
Maintain model cards, changelogs, and version control so auditors can trace how information and assumptions shaped outcomes.
Due process and recourse: Clear explanations, appeals, and beneficiary rights
“People must receive plain-language notices, timely appeals, and access to a human reviewer.”
Guarantee human-in-the-loop checkpoints and require written override rationales. Transparent appeal paths protect rights and preserve trust.
Privacy-by-design: Data minimization, access controls, and accountability
Embed privacy practices: collect only needed data, enforce role-based access, and log every automated recommendation. Regular audits ensure the system respects privacy and holds staff accountable.
- Practical guide: Bake fairness into algorithmic decision-making and publish research findings.
- Operational rule: Tools must include human review, monitoring for drift, and documented remedies when harms appear.
- Governance aim: Align oversight with solutions that protect benefits and sustain public trust, with independent review to verify compliance.
Stakeholder perspectives: Individuals, families, agencies, and solution providers
Voices from households and front-line workers reveal how policy decisions touch everyday routines. Stakeholders describe outcomes in human terms: lost hours of care, surprise notices, and weeks of paperwork that upend life.
People and families want clarity and a fair way to challenge results. They need notices that explain why a decision happened and the steps to appeal.
Agencies and organizations aim to protect program integrity while honoring each person’s circumstances. Caseworkers need tools that explain recommendations and preserve care continuity.
Solution providers must design interfaces with empathy so beneficiaries are empowered, not overwhelmed.
Balancing organizational goals with the lives of beneficiaries
- Surface perspectives from people and families affected by daily care and financial stability.
- Reward accuracy and fairness in organizational incentives, not just detection volume.
- Use transparent algorithms and clear escalation paths so practitioners can make humane adjustments.
“A people-first approach balances program safeguards with dignity and autonomy.”
| Stakeholder | Primary need | Operational implication |
|---|---|---|
| People & families | Clear notices and fast appeals | Reduce wrongful disruption to care |
| Caseworkers | Explainable recommendations | Faster, fairer decisions |
| Agencies & organizations | Integrity and access balance | Policies that prevent harm while reducing waste |
| Solution partners | Design with empathy | Interfaces that empower individuals |
Conclusion
Closing this review, the path ahead centers on durable oversight and humane outcomes. Agencies can pair operational excellence with clear safeguards so benefits and care are preserved for each person.
Today’s leaders have a way forward: mandate fairness testing, publish plain-language notices, and provide rapid appeals. These steps protect life, reduce wrongful flags, and keep systems accountable.
Practical success is measured by real outcomes — days of care maintained, appeals resolved, and trust sustained — not just dollars flagged. The welfare ecosystem will improve when agencies share methods, monitor impact, and correct course quickly.
At the end, resilient policy and human oversight make the difference. For more context on harms and reform lessons, see this welfare benefits review.
FAQ
What does this case study cover and why does it matter today?
This case study examines how automated models are used to identify suspect claims and reduce waste in social benefit programs. It matters because systems touch millions of beneficiaries, can change access to care and income, and carry risks for privacy, fairness, and due process. The study highlights operational wins, real-world harms, and governance lessons for safer deployment.
Who is affected by large-scale fraud detection systems in social benefits?
Programs that serve tens to hundreds of millions of people can be affected: beneficiaries, families, providers, agency staff, and third‑party vendors. When models make or support decisions, individuals seeking health care, disability support, or income can face reduced benefits, wrongful accusations, or delayed assistance.
What types of data do these systems typically use and who can access it?
Systems draw on claims records, beneficiary demographics, provider information, assessment responses, and administrative logs. Access is usually limited to agency staff, contracted vendors, and sometimes auditors; however, insufficient controls and data sharing agreements can expose sensitive information and increase privacy risk.
How do the models work — are they simple rules or machine learning?
Deployments range from rule-based scoring to statistical classifiers and hybrid models that combine rules with machine learning. Many systems use pattern detection, anomaly scoring, and risk thresholds; others incorporate subject-matter features and human review to reduce false positives.
What scale and throughput do modern systems handle?
Some national systems cover over 160 million people and process millions of claims per day. High throughput demands automation for triage and prioritization, which in turn raises stakes for accuracy, latency, and monitoring at scale.
What operational benefits have organizations reported?
Agencies and vendors report faster model development cycles, improved triage, and higher precision in flagged cases. In certain deployments, teams reduced model development time from months to minutes and reported detection precision above 90%, enabling quicker investigations and workload reductions.
What measurable financial outcomes have resulted from these systems?
Some programs have identified over
FAQ
What does this case study cover and why does it matter today?
This case study examines how automated models are used to identify suspect claims and reduce waste in social benefit programs. It matters because systems touch millions of beneficiaries, can change access to care and income, and carry risks for privacy, fairness, and due process. The study highlights operational wins, real-world harms, and governance lessons for safer deployment.
Who is affected by large-scale fraud detection systems in social benefits?
Programs that serve tens to hundreds of millions of people can be affected: beneficiaries, families, providers, agency staff, and third‑party vendors. When models make or support decisions, individuals seeking health care, disability support, or income can face reduced benefits, wrongful accusations, or delayed assistance.
What types of data do these systems typically use and who can access it?
Systems draw on claims records, beneficiary demographics, provider information, assessment responses, and administrative logs. Access is usually limited to agency staff, contracted vendors, and sometimes auditors; however, insufficient controls and data sharing agreements can expose sensitive information and increase privacy risk.
How do the models work — are they simple rules or machine learning?
Deployments range from rule-based scoring to statistical classifiers and hybrid models that combine rules with machine learning. Many systems use pattern detection, anomaly scoring, and risk thresholds; others incorporate subject-matter features and human review to reduce false positives.
What scale and throughput do modern systems handle?
Some national systems cover over 160 million people and process millions of claims per day. High throughput demands automation for triage and prioritization, which in turn raises stakes for accuracy, latency, and monitoring at scale.
What operational benefits have organizations reported?
Agencies and vendors report faster model development cycles, improved triage, and higher precision in flagged cases. In certain deployments, teams reduced model development time from months to minutes and reported detection precision above 90%, enabling quicker investigations and workload reductions.
What measurable financial outcomes have resulted from these systems?
Some programs have identified over $1 billion in suspect claims annually. Savings claims vary by jurisdiction and depend on follow‑up, adjudication quality, and whether identified cases lead to recoveries or prevented improper payments.
What harms and risks have been documented?
Documented harms include discriminatory outcomes by age, disability, marital status, and nationality; wrongful benefit reductions; opaque decision-making; and procedural failures that deny timely appeal. System errors and misapplied software have led to reputational and legal consequences in multiple countries.
How do fairness and bias issues typically appear in these systems?
Bias appears when training data reflect historical inequalities, when variables correlate with protected characteristics, or when thresholds disproportionately affect subgroups. Without targeted fairness testing and mitigation, disparities in outcomes become statistically significant and practically harmful.
What governance measures reduce these harms?
Effective measures include clear problem definitions (fraud vs. error), documented data lineage, regular fairness testing, human-in-the-loop review, red‑teaming, and accessible appeal processes. Privacy-by-design, access controls, and transparent reporting further improve accountability.
What lessons can be drawn from international failures like the Netherlands and Australia?
High-profile failures show the cost of automation without due process: wrongful accusations, legal challenges, and large repayments. These cases underscore the need for legal safeguards, independent audits, and meaningful human oversight before scaling automated decisions.
How should agencies balance efficiency with the human impact of automated decisions?
Agencies should set proportional responses: use automation for triage and prioritization, preserve human review for adverse actions, and design recourse channels that are fast and accessible. Combining subject-matter expertise with analytics produces more defensible outcomes.
What role do vendors and contractors play, and how should they be held accountable?
Vendors often supply models, software, and operational capacity. Contracts must require transparency, audit rights, documented validation, and obligations for ongoing monitoring. Public agencies should retain oversight and the ability to contest vendor findings.
How can beneficiaries challenge or appeal automated findings?
Best practice requires clear notice when automation influences a decision, plain-language explanations of the rationale, and timely, funded appeal mechanisms with access to human adjudicators. Without these safeguards, automated processes risk violating due process.
What immediate steps should leaders take when implementing these systems?
Leaders should map stakeholders and risks, run pilot studies with independent audits, implement privacy and access controls, require continuous performance monitoring, and codify appeals and redress procedures before full rollout.
Which disciplines should be involved in building responsible systems?
Multidisciplinary teams work best: data scientists, policy experts, social workers, legal counsel, ethicists, and affected-community representatives. This mix ensures technical soundness and alignment with human-rights, privacy, and program goals.
Where can leaders find practical frameworks for oversight and fairness testing?
Leaders can draw on peer-reviewed research, government guidance from agencies such as the U.S. Office of Management and Budget, and frameworks published by standards bodies and civil-society organizations. Independent audits and published fairness assessments help translate principles into practice.
billion in suspect claims annually. Savings claims vary by jurisdiction and depend on follow‑up, adjudication quality, and whether identified cases lead to recoveries or prevented improper payments.
What harms and risks have been documented?
Documented harms include discriminatory outcomes by age, disability, marital status, and nationality; wrongful benefit reductions; opaque decision-making; and procedural failures that deny timely appeal. System errors and misapplied software have led to reputational and legal consequences in multiple countries.
How do fairness and bias issues typically appear in these systems?
Bias appears when training data reflect historical inequalities, when variables correlate with protected characteristics, or when thresholds disproportionately affect subgroups. Without targeted fairness testing and mitigation, disparities in outcomes become statistically significant and practically harmful.
What governance measures reduce these harms?
Effective measures include clear problem definitions (fraud vs. error), documented data lineage, regular fairness testing, human-in-the-loop review, red‑teaming, and accessible appeal processes. Privacy-by-design, access controls, and transparent reporting further improve accountability.
What lessons can be drawn from international failures like the Netherlands and Australia?
High-profile failures show the cost of automation without due process: wrongful accusations, legal challenges, and large repayments. These cases underscore the need for legal safeguards, independent audits, and meaningful human oversight before scaling automated decisions.
How should agencies balance efficiency with the human impact of automated decisions?
Agencies should set proportional responses: use automation for triage and prioritization, preserve human review for adverse actions, and design recourse channels that are fast and accessible. Combining subject-matter expertise with analytics produces more defensible outcomes.
What role do vendors and contractors play, and how should they be held accountable?
Vendors often supply models, software, and operational capacity. Contracts must require transparency, audit rights, documented validation, and obligations for ongoing monitoring. Public agencies should retain oversight and the ability to contest vendor findings.
How can beneficiaries challenge or appeal automated findings?
Best practice requires clear notice when automation influences a decision, plain-language explanations of the rationale, and timely, funded appeal mechanisms with access to human adjudicators. Without these safeguards, automated processes risk violating due process.
What immediate steps should leaders take when implementing these systems?
Leaders should map stakeholders and risks, run pilot studies with independent audits, implement privacy and access controls, require continuous performance monitoring, and codify appeals and redress procedures before full rollout.
Which disciplines should be involved in building responsible systems?
Multidisciplinary teams work best: data scientists, policy experts, social workers, legal counsel, ethicists, and affected-community representatives. This mix ensures technical soundness and alignment with human-rights, privacy, and program goals.
Where can leaders find practical frameworks for oversight and fairness testing?
Leaders can draw on peer-reviewed research, government guidance from agencies such as the U.S. Office of Management and Budget, and frameworks published by standards bodies and civil-society organizations. Independent audits and published fairness assessments help translate principles into practice.