Ever notice when a conversation suddenly stops? Maybe a parent can’t hear their child laugh. Or a founder misses important cues in a meeting. These quiet moments can really affect our confidence and how well we work.
Telehealth teleaudiology services aim to fix this. They bring hearing care right to your home, office, or even rural clinics. This way, you can hear clearly again.
This guide is for anyone in hearing care. It shows how digital services can help, not just replace, face-to-face visits. You’ll learn how to set up virtual consultations and fit hearing aids remotely. It also shares tips on making sure patients are ready and how to keep their information private.
It talks about what you need to start: a good computer, internet, and clear sound. It also stresses the importance of the doctor’s skills. You’ll learn how to get ready, like checking licenses and using safe online tools.
Key Takeaways
- Telehealth teleaudiology services expand access while complementing in-person care.
- Digital hearing health services require both patient readiness and clinician training.
- Telehealth hearing aid fittings can be effective with proper technology and privacy safeguards.
- Virtual audiology consultations rely on HIPAA-compliant platforms and clear workflows.
- Adoption succeeds when systems address equipment, licensure, and patient education.
Understanding Telehealth Teleaudiology Services
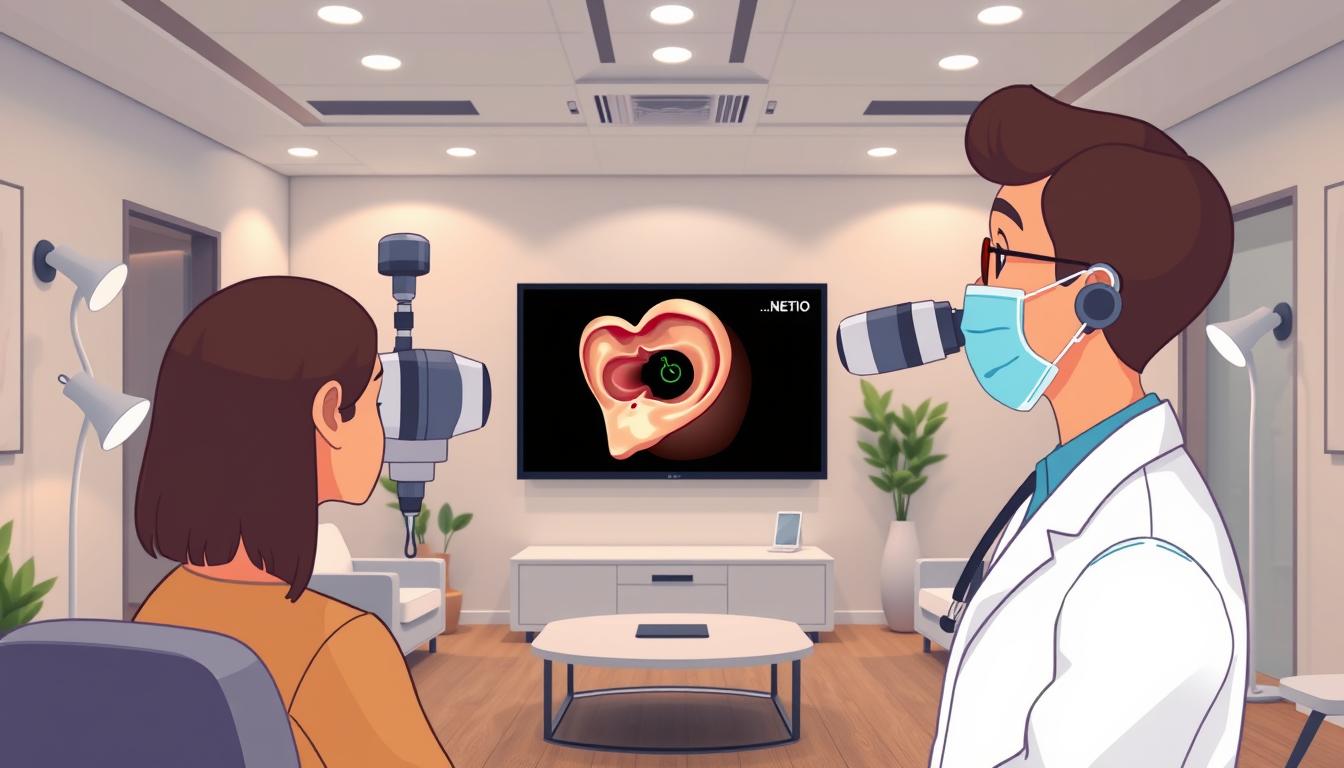
Teleaudiology is where audiology meets modern tech. It lets audiologists help patients from afar. They can do many things, like check hearing and adjust devices.
Definition and Scope
Telehealth teleaudiology means getting hearing care online. You can get virtual audiology checks and hearing tests from home. This is great for those who can’t go to a clinic.
Services include fitting hearing aids and speech therapy online. These help when you can’t see a doctor in person. They’re good for people in remote areas or during health crises.
Doctors use rules to know when to use telehealth. They check if it’s safe and if the patient is okay. This includes knowing when to see a patient in person.
The Role of Technology in Teleaudiology
Technology makes it all work. Tools like FaceTime and Zoom are used with care. You need a good internet and clear sound.
Doctors need to test and fix tech issues. They also learn how to use it for remote care. This ensures care is consistent.
It’s important for patients to be ready too. Easy-to-use tech and clear instructions help. Keeping data safe and getting consent is also key.
When tech, doctors, and patients are all ready, teleaudiology works well. It keeps care going online. This makes hearing care more accessible without losing quality.
Benefits of Telehealth Teleaudiology Services
Remote care has big benefits for those needing hearing help. It cuts down on travel and missed appointments. All you need is a phone, internet, and simple audio tools to start.
Enhanced Accessibility for Patients
People in rural areas and those who can’t move easily get help faster. Clinics in Alaska and other far places now offer care online. This means no long trips for many.
Doctors learn to help those who don’t know how to use tech. This makes everyone feel more comfortable. Some patients get a face-to-face visit first, then online check-ups. This way, they get the care they need without leaving home.
During the pandemic, many stayed away from clinics. But telehealth reached 32.8% of those who might have missed out. It uses tools like mobile otoscopy and portable audiometers for accurate tests. This helps those who are hard to reach as shown in studies.
Improved Patient Engagement and Satisfaction
Patients love the ease of online follow-ups. They’re happy with hearing aid tweaks done from afar. This keeps care on track and encourages regular visits.
Doctors get better at telehealth with practice. This makes patients happier. Even though some like in-person visits, online options are a big win for everyone.
- Access: Expands reach to rural and mobility-limited populations.
- Convenience: Reduces travel time and missed appointments.
- Engagement: Enables frequent, timely touchpoints for better outcomes.
- Scalability: Integrates with in-person care for a hybrid model.
How Teleaudiology Works
Teleaudiology mixes technology with expert care. It brings hearing help to homes and clinics. A clear plan guides each step, from booking to follow-ups.
This method makes care easy and safe. It lets doctors decide when to see patients in person.
The Patient Journey in Teleaudiology
Before the visit, steps are set to make things clear. Patients call or email to check on details. They confirm the doctor’s license, tech needs, insurance, costs, and privacy.
Doctors send simple instructions before the visit. They talk about timing, how to set up devices, and what to do if problems arise.
During the visit, doctors take a detailed history. They use video otoscopy and do remote hearing checks. They also fit hearing aids through apps and Bluetooth.
After the visit, doctors write down what happened. They plan for follow-ups and check on patients remotely. They have plans for emergencies and keep care going smoothly.
Tools and Platforms Used in Teleaudiology
Doctors pick tools and platforms based on what they need and what patients can use. They might use FaceTime, Zoom, or Google Meet. Or they might use special telehealth portals that keep things private.
For remote care, doctors use video otoscopes and special software. They also use hearing-aid apps from companies like Phonak and Oticon. These apps let them adjust hearing aids remotely.
Teams learn how to use and fix equipment. They practice for when things go wrong. This helps keep sessions going without trouble.
For more info on teleaudiology, check out this review: teleaudiology review. The success of teleaudiology depends on good planning, the right tools, and careful follow-up.
Regulatory Landscape Governing Teleaudiology
Rules shape teleaudiology’s growth in the U.S. Providers, clinics, and patients face privacy rules, licensure limits, and more. Clear rules help teams offer safe, compliant services that meet patient needs.
Key Legislation Impacting Telehealth
Federal law sets basic protections. HIPAA ensures secure platforms and privacy for remote care. Patients should check if a platform is HIPAA-compliant before sharing info.
Clinicians must know their scope of practice for remote work. This is important under current rules.
Organizational strategy is key. Health systems need to define roles and train staff. They should adopt standards for allied health professions.
Legal details affect feasibility. Rules on billing, scope of practice, and licensure influence program growth. Teams should document policies to align with changing rules.
State-Specific Regulations and Requirements
Licensure is critical. Clinicians must check licensure requirements before treating patients across state lines. Some states have easier rules, while others are stricter.
Training and documentation standards vary by state. Telehealth training should meet state expectations. Providers must stay updated on state rules.
Reimbursement and coverage vary by payer and state. Patients and providers should check if a tele-visit is covered. Clear billing protocols help with claims and patient understanding.
The key takeaway is to align platforms with HIPAA and check licensure for each patient. Build protocols that reflect state rules. Investing in competency and legal review reduces risk and supports quality care.
| Regulatory Area | What Providers Must Do | Patient Action |
|---|---|---|
| Privacy & Security (HIPAA) | Use HIPAA-compliant platforms; train staff on secure workflows | Ask if platform is HIPAA-compliant; verify data protections |
| Licensure & Scope | Confirm state licenses or compact eligibility before each tele-visit | Verify provider is licensed for audiology or hearing-aid services in their state |
| Workforce Competency | Adopt telehealth competency standards and role definitions | Request information on provider training and teleaudiology experience |
| Reimbursement & Coverage | Document billing rules and confirm payer policies by state | Check insurance coverage and possible costs |
| State Rules & Boards | Monitor state board updates and update protocols as needed | Ask about following state-specific telehealth rules and documentation |
Finding a Teleaudiology Provider
Choosing the right teleaudiology partner is important. Look for licensure, platform security, and technical fit. Also, check if they have proven training.
It’s key to find a provider that is safe and effective for all ages.
Tips for Locating Qualified Professionals
Start with professional directories like the American Speech-Language-Hearing Association. They list clinicians who offer telehealth services and show their credentials.
Check clinic websites and hospital portals for virtual audiology details. Look for remote hearing-aid support. Vendor programs show which hearing aids can be adjusted remotely.
Choose providers with formal telehealth training. Programs with telehealth curricula report better patient safety and smoother visits.
- Verify use of a HIPAA-compliant telehealth platform.
- Look for experience with remote hearing-aid adjustments and curbside repair options.
- Confirm the team has documented telehealth training or affiliation with academic programs.
Questions to Ask Potencial Providers
Ask if the audiologist or hearing-aid dispenser is licensed for telehealth in your state. Licensing rules vary and affect care.
- What hardware and software are needed for virtual audiology consultations? Is the platform HIPAA-compliant?
- Can my Bluetooth hearing aids connect to your system for remote adjustments? What app is needed?
- What services can you deliver remotely—hearing tests, otoscopy, hearing-aid programming?
- Is the tele-visit private and covered by insurance? What will out-of-pocket charges be?
- What if the connection fails? Do you offer curbside repair or in-person escalation?
- What telehealth training does your team have? Can you share patient outcomes related to telehealth speech therapy or remote audiology care?
A comparison table helps when choosing a teleaudiology provider. It scores licensure, tech compatibility, training, and contingency planning.
| Evaluation Area | What to Look For | Why It Matters |
|---|---|---|
| Licensure | State authorization for telehealth audiology | Ensures legal practice and continuity of care across state lines |
| Platform Security | HIPAA-compliant video and data transfer | Protects patient privacy during virtual audiology consultations |
| Technical Compatibility | Support for Bluetooth hearing aids and required apps | Allows remote adjustments and reduces need for in-person visits |
| Telehealth Training | Formal coursework or simulation experience | Improves clinical outcomes and patient safety in telehealth teleaudiology services |
| Services Offered | Remote testing, otoscopy, programming, and telehealth speech therapy links | Defines scope of care and whether needs can be met virtually |
| Cost and Coverage | Clear fees, insurance acceptance, and billing for tele-visits | Prevents surprises and supports informed decision-making |
| Contingency Plans | Curbside repair, escalation to in-person care, backup contact methods | Maintains care when technology or access fails |
Use these questions during outreach and intake calls. Careful vetting reduces delays and improves outcomes with telehealth services.
Challenges and Limitations of Teleaudiology
Telehealth services make care easier to get. But, there are big challenges. These can make remote hearing tests not as good as they should be.
Technical Barriers and Solutions
Patients often don’t have the right tools. They might not have a recent device or good internet. They might not know how to use video calls.
To fix this, ask patients to use a recent laptop or phone. Do a quick tech check before the visit.
Using the right equipment helps a lot. Suggest headsets and hearing aids that stream sound. Make sure patients are in a quiet place.
When tech fails, have backup plans. Use low-bandwidth options and messaging. This keeps care going.
Doctors need to learn how to fix tech problems. They should know how to handle bad audio and disconnections. Training that mixes real practice with simulation helps doctors feel ready.
Some patients are scared because they don’t know what to expect. Teach them step by step. Offer chat or messaging as options. Studies show that clear instructions help patients feel more comfortable.
Learn more about teleaudiology challenges and solutions in this review here.
Patient Privacy and Data Security Concerns
Keeping patient info safe is key in telehealth. Use secure platforms and be open about how you handle data. Always get consent before recording or sharing data.
Doctors need to know how to protect privacy. They should understand software rules and ensure EHRs are used safely. Avoid apps that don’t protect data well.
There are real risks like data leaks from unsafe platforms. Choose good platforms, get clear consent, and have plans for emergencies. This builds trust and makes telehealth work.
To solve these problems, we need to train doctors and teach patients. We also need secure tech and clear consent. These steps help keep care quality high and make remote hearing tests work well.
The Future of Telehealth Teleaudiology Services
Remote hearing care is changing. Now, clinics mix in-person visits with online follow-ups. They use curbside repairs and apps for hearing aid fittings.
This shift is part of a bigger trend in teleaudiology. It’s also seen in speech therapy and other services.
New tech will soon allow for remote tests and video exams. Training for telehealth is becoming common. Clinicians need to learn how to use these new tools safely.
Investing in patient education and clinic setup is key. This will help us move past the early days of telehealth.
Trends and Innovations in Teleaudiology
Remote tests are getting better. Now, clinicians can adjust hearing aids and screen patients online. This lets them help more people without losing quality.
Tools for remote care are getting better. They work even in areas with slow internet. Training teams to work with these tools is important.
More people will use teleaudiology if we fix a few things. We need better payment, training, and education for patients.
The Role of Artificial Intelligence and Machine Learning
AI is making teleaudiology better. It helps with hearing tests and makes care more personal. AI can also help doctors make decisions faster.
But, we need to make sure AI is used right. Clinicians must learn to use it safely. We also need to be open about how AI works and keep patient data safe.
For AI to help, we need good tech, training, and rules. When we have these, teleaudiology can offer better care. It will be more personal and safe for everyone.
Comparisons: Teleaudiology vs. Traditional Audiology
Telehealth and in-person clinics both aim to help with hearing. They do this through diagnosis, treatment, and more. But, they do it in different ways.
Both need good communication and knowledge. Telehealth also needs technical skills. This includes setting up online meetings and using the right tools.
Similarities and Differences
Both methods assess patients and track progress. But, teleaudiology is more accessible. It saves time and money for patients.
Some patients prefer to see a doctor in person. A study in Saudi Arabia found 80.2% of patients like face-to-face visits.
Clinics adjust to new ways of working. Remote visits are good for many things. But, some tasks need to be done in person.
Cost Effectiveness in Treatment Options
Teleaudiology can save money for both patients and clinics. It cuts down on travel costs and makes care more accessible.
Starting up teleaudiology might cost money. But, it can make care more efficient over time. It’s important to check if insurance covers these services.
Teleaudiology and in-person care work together. Remote visits are great for many tasks. But, some things need to be done in a clinic.
Patient Testimonials and Case Studies
Telehealth teleaudiology services are both useful and focused on patients. Many patients are happy with remote hearing-aid adjustments and Bluetooth streaming. They find it works well once they get used to it.
Follow-ups, quick fixes, and app-based updates solve problems fast. This is better than waiting for in-person visits.
Success Stories from Teleaudiology Patients
Real stories show how teleaudiology works well. It helps with hearing aid fine-tuning, quick fixes, and keeps care going even when clinics are closed. Training programs in the U.S. also help doctors get better at virtual care.
Even in other places, people like it because it keeps them away from clinics during crises.
Lessons Learned from Real-World Applications
Getting things right is key. Prepare patients with guides, tell them what they need, and have backup plans. Training doctors well helps them feel confident and safe.
Make sure everything is private and clear about costs. This way, teleaudiology can help a lot with follow-ups and managing devices. It shows how to make virtual care better for everyone.
FAQ
What are telehealth teleaudiology services and how do they differ from in‑person audiology?
Telehealth teleaudiology services let you get audiology care from home. You can do video calls, hearing tests, and even get your hearing aids adjusted online. It’s not a full replacement for in-person visits, but it’s a big help.
Some things like follow-ups and fine-tuning work well online. But, some tests need you to be there in person.
What technology do patients need for a successful virtual audiology visit?
You’ll need a smartphone or laptop with a good camera, fast internet, and speakers or a headset. If you have Bluetooth hearing aids, you can stream audio directly. Your audiologist might use special tools and apps to help.
They’ll also have backup plans to keep things running smoothly.
Are consumer platforms like Zoom, FaceTime, or Google Meet acceptable for teleaudiology?
Yes, you can use platforms like Zoom or FaceTime if they’re secure. But, your audiologist might prefer apps that are made for health care. Make sure to ask about the safety of the platform they choose.
How should clinicians and clinics prepare patients before a teleaudiology visit?
Your audiologist should check if they’re licensed and explain what you need for the visit. They’ll also talk about insurance and give you instructions on how to get ready. A quick tech check call can help too.
For hearing aid fittings, make sure you know which app to use and how to connect your devices.
What competencies should clinicians have for effective teleaudiology care?
Audiologists need to know when to use telehealth and how to communicate well over video. They should also be tech-savvy and know how to fix problems. Training is key to being good at teleaudiology.
How does teleaudiology improve access and convenience for patients?
Teleaudiology saves you from having to travel and is great for people who can’t get to the clinic easily. It’s also good for quick follow-ups and adjusting your hearing aids without having to meet in person.
But, it works best if you and your audiologist are ready and if the technology is good.
Do patients accept teleaudiology and are they satisfied with remote hearing‑aid adjustments?
Some patients like getting their hearing aids adjusted online, but others prefer to see their audiologist in person. It really depends on the person.
Showing them how it works and making sure they’re comfortable with it can help.
What privacy and data security issues should patients ask about?
Ask if the platform is safe and if they keep your data private. Find out if they record sessions and how they handle your information. It’s also important to know if they have a plan for keeping your data safe.
How do licensure and state regulations affect access to teleaudiology?
Your audiologist needs to be licensed in your state to practice teleaudiology. The rules can vary, so it’s good to ask about them. Insurance coverage also depends on where you live and what services you need.
Will insurance cover teleaudiology visits and remote hearing‑aid services?
Insurance coverage for teleaudiology varies. Some plans cover it, while others don’t. It’s best to check with your insurance company and talk to your audiologist about costs.
How can patients locate qualified teleaudiology professionals?
Look for audiologists who offer teleaudiology services and use safe platforms. Check professional directories like the American Speech-Language-Hearing Association (ASHA) and the American Academy of Audiology (AAA). You can also search online or ask for recommendations.
What questions should patients ask prospective teleaudiology providers?
Ask about their licensure, if they follow privacy rules, what technology they use, and if they can help with your hearing aids. Also, find out if they’re covered by your insurance and what you’ll need to do before your visit.
What common technical barriers occur and how are they resolved?
Problems like old devices, slow internet, and not knowing how to use the platform can happen. To fix these, use modern devices, good internet, and headsets. Your audiologist should also check your tech before your visit.
They might have backup plans or ways to make things easier for you.
What innovations are shaping the future of teleaudiology?
New things like better platforms, remote tests, and tools that use AI are coming. These will make teleaudiology even better. Training for audiologists and more access to these services will help everyone.
How might AI and machine learning be used in remote hearing care?
AI can help with early tests, making hearing aids better, and helping decide when you need to see an audiologist in person. But, it needs to be tested and used carefully. Your audiologist should explain how it works and its limits.
In what scenarios should teleaudiology escalate to in-person care?
If online tests aren’t clear, if you need a full check-up, or if there’s a tech problem, you might need to see your audiologist in person. Your audiologist will know when it’s best to see you face-to-face.
Is teleaudiology cost-effective?
Teleaudiology can save you money by cutting down on travel and no-shows. It’s also good for quick adjustments to your hearing aids. But, it might cost more upfront for the technology and training.
It really depends on how often you use it and if your insurance covers it.
What real-world lessons improve teleaudiology implementation?
To make teleaudiology work well, prepare patients, train audiologists, and use easy-to-use platforms. Make sure to follow privacy rules and have ways for patients to communicate. Early adopters should share their experiences to help others.