In hospital corridors, time seems to move slowly, just like the patients. Clinicians and families often see long waits and repeated tests. They feel the weight of chronic illness.
For those who care deeply, these moments are a call to action. How can AI in healthcare ease the strain? How can it give back time to doctors and improve patient outcomes?
Artificial intelligence in healthcare is real and changing care today. It uses advanced tools to find patterns in data and understand clinical notes. It even helps classify images.
Investments in data centers and special chips are making AI more powerful. This lets AI help doctors and patients in real ways.
Early uses of AI are showing great results. Diagnoses are faster, workflows are smoother, and resources are used better. Oracle Health is a great example, with tools that help doctors talk to patients and analyze data.
But, there’s a big responsibility with AI. Data quality, governance, and trust from doctors are key. They help make AI’s promise a reality.
Key Takeaways
- AI-powered medical advancements address systemic strains like aging populations and rising chronic disease costs.
- Artificial intelligence in healthcare relies on large datasets, neural networks, and specialized infrastructure.
- Practical uses already include diagnostic support, risk prediction, and operational efficiencies.
- Clinical risk reduction—such as medication safety and fall prediction—is a major benefit when implemented carefully.
- Real-world platforms like Oracle Health illustrate enterprise adoption and the need for governance.
- Leaders must invest in data quality and clinician trust to realize strategic value from the ai in healthcare sector.
Introduction to AI in Healthcare
Artificial intelligence is changing healthcare in big ways. It’s making clinical work, research, and patient care better. This intro explains what AI in healthcare is and why it’s important.
Definition of AI in Healthcare
AI in healthcare includes many tools like machine learning and deep learning. These tools help doctors by looking at health records and images. They also help with making decisions.
AI uses big data to learn and then answers questions. It can be updated or changed. This makes it better for solving tough health problems.
Importance of AI in Modern Healthcare
Healthcare faces big challenges like aging people and not enough doctors. AI offers a solution by making work easier and helping patients more. It’s a big help when used right.
Studies show AI can spot problems like falls and medication mistakes. But, making AI work well in healthcare is hard. Leaders need to work on making data work together better.
AI can help doctors spend more time with patients. It can write notes and make charts easier. But, making sure data is good and safe is key. Standards like mCODE help make research and AI work better together.
Benefits of AI for Patient Care
AI tools are changing how doctors find diseases, plan treatments, and care for patients. Systems that use clinical data, images, and patient reports can speed up diagnosis. This helps busy teams work better.
Enhanced Diagnosis Accuracy
AI in healthcare has made finding diseases in scans better. It spots areas likely to have problems. This lets doctors act early to protect patients.
AI helps doctors make better decisions in tough cases. Studies show AI-assisted readings are better than without AI. This means fewer missed diagnoses and faster care.
AI also finds problems that are not reported. It looks at reports and finds patterns. This makes audits easier and keeps patients safer.
Personalized Treatment Plans
AI helps tailor treatments to each patient. It uses genetics, health history, and past treatments. This makes treatments more effective.
In clinical trials, AI finds groups that benefit from treatments. This helps make treatments more precise. It’s good for cancer and chronic diseases.
AI also helps with remote care. It uses wearables and chatbots to keep patients on track. This makes care plans more effective.
| Area | AI Role | Typical Impact |
|---|---|---|
| Medical Imaging | Automated lesion detection and volume measurement | Earlier detection; reduced radiologist review time |
| Clinical Decision Support | Case-specific suggestions from ML models | Higher diagnostic accuracy; faster triage |
| Safety Surveillance | NLP-based incident detection and classification | Improved adverse event capture; fewer manual audits |
| Precision Therapeutics | Genomic and EHR-driven dosing models | Better outcomes; reduced adverse reactions |
| Remote Care | Virtual assistants and wearable analytics | Improved adherence; timely plan adjustments |
| Administration | Automated scheduling and prior authorization | Lower operational burden; higher patient engagement |
Studies from 2007 to 2024 show AI’s benefits. It helps find diseases, prevent problems, and makes work easier. AI is useful when used right. It helps patients and doctors a lot.
AI Applications in Clinical Settings
Clinical teams use special tools to act fast on data. These tools help predict risks, support diagnoses, and sort tasks. They work well with electronic medical records.
Predictive Analytics for Patient Outcomes
Predictive systems forecast falls, readmissions, and bad events. They use advanced models like neural networks. Studies show these models are very accurate.
They help staff focus on high-risk patients. This way, they can use resources better. When doctors use these predictions, they see fewer bad events.
AI makes clinical trials faster. It finds the right patients and spots problems. This makes trials safer and more efficient.
AI-Assisted Diagnostics
AI helps doctors by pointing out important areas on scans. This makes doctors better at finding problems. Companies like GE Healthcare make these tools easy to use.
NLP looks through notes to find important info. It helps doctors catch problems early. This makes care safer and better.
AI suggests possible diagnoses and what tests to do next. Doctors see it as a helpful tool. It helps them make better decisions.
For AI to work well, data must be clean and organized. Teams need to train and guide each other. This way, AI helps doctors more effectively.
Role of AI in Medical Imaging
Medical imaging has changed a lot. Now, machines help read scans fast and right every time. Doctors use special tools that mix two kinds of models to spot small details on scans.
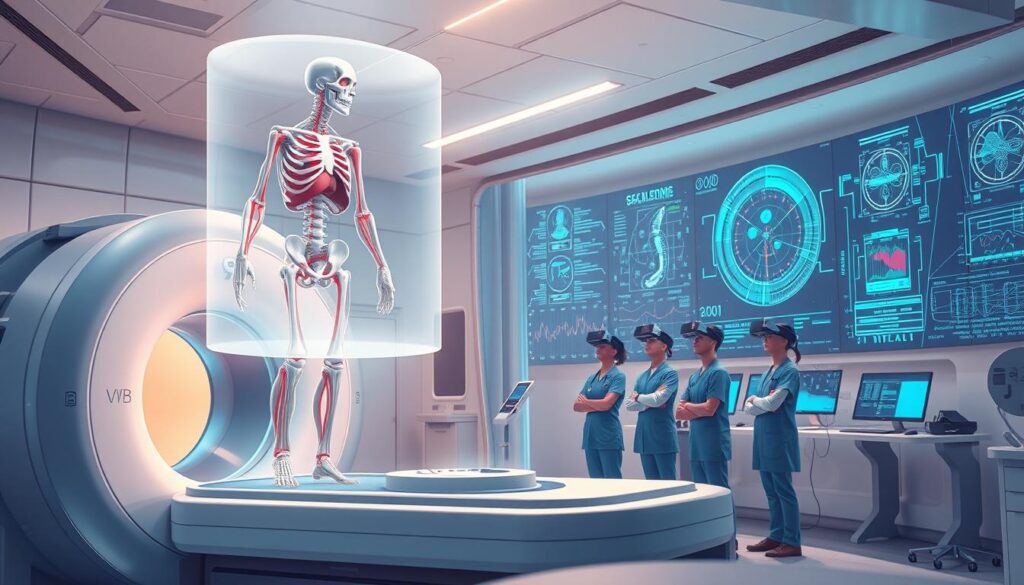
Image Recognition and Analysis
Deep learning models find things that humans might miss. They look at changes in organs and find important signs early. This helps doctors act fast when it’s really important.
Systems now sort scans to find the most urgent ones first. This makes reports come back quicker. Doctors say they can read scans faster and more accurately.
For more info, check out this medical imaging research review on PubMed Central.
Reduction of Human Error
AI helps catch small changes and misses. This means doctors can find problems sooner. It also gives teams clear data to work with.
It’s important to test AI on many kinds of data. This makes sure it works well everywhere. When used right, AI frees up doctors to focus on what really matters.
AI in Drug Discovery and Development
The world of drug discovery is changing fast. AI tools are moving from test projects to real use. Researchers and biotech leaders use AI to screen compounds and predict how they work.
AI looks through huge libraries of molecules to find new ideas. It spots patterns that humans might miss. This helps find the best compounds faster and cuts down on failures later on.
Clinical development gets better with AI too. AI picks the right patients for trials. This makes studies more effective and saves money.
Accelerating the Drug Development Process
AI makes drug development faster by doing routine tasks. It helps decide which experiments to do first. This means teams can make decisions quicker and work more efficiently.
AI also helps understand how drugs work and their safety. This information helps plan better trials. It lets drug developers make their work more focused and effective.
Cost-Effectiveness in Research
AI helps save money in research. It picks the most promising compounds to test. This means fewer tests are needed, saving time and money.
AI also predicts problems early on. This lowers the risk of expensive failures later. It helps keep patients safe and saves money for drug companies.
For entrepreneurs and R&D leaders, the message is clear. Start building strong data pipelines and testing frameworks early. When AI is used well, it can make research faster and cheaper.
| Area | AI Role | Practical Impact |
|---|---|---|
| Molecular Screening | Predict binding, prioritize scaffolds | Reduces candidate pool, focuses lab resources |
| Preclinical Safety | Forecast toxicity signals | Lowers chance of late-stage failure |
| Trial Design | Identify responders, optimize cohorts | Improves statistical power, shortens timelines |
| Post-Market Surveillance | Detect adverse-event patterns across demographics | Targets safety reviews, informs labeling |
| Decision Strategy | Integrate multi-source evidence for go/no-go | Enables faster commercialization choices |
Telemedicine and AI Integration
Telemedicine has grown beyond just video calls. It now uses smart tech to help patients from anywhere. Hospitals and startups use tools to make care easier and find important health clues from data.
AI-driven virtual health assistants
Chatbots and virtual helpers do simple tasks like scheduling and reminding you to take medicine. They help doctors focus on harder cases. This makes patients more involved and follow their care plans better.
It’s important to make sure these tools are safe. They should not give bad advice and have ways to get help from doctors. Tests show that voice recognition is promising but need careful checks and training for doctors.
- Common functions: triage advice, reminders, scheduling.
- Safety guardrails: escalation triggers, clinician review, rigorous validation.
- Deployment tip: phase pilots within existing workflows to build clinician trust.
Remote monitoring and support
Wearables and sensors send health data all the time. AI spots problems early and helps quickly. This is good for heart issues, diabetes, and cancer care.
Studies show early detection and quick action can help patients. Successful programs have clear alerts and specific roles for nurses and doctors.
- Data sources: smartwatches, glucose monitors, cardiac patches, bedside telemetry.
- Clinical value: early warning, readmission risk prediction, targeted outreach.
- Operational need: interoperability standards and robust data governance.
Operational benefits and practical caution
AI helps bring expert care to places that need it most. It sends reminders and flags risks to keep people healthy. This helps reduce missed appointments.
Remote care helps predict problems like falls and bad reactions. But, it needs to keep patient data safe and work with different devices. Doctors must also trust and use these tools.
Many projects start small and work well. But, to grow, they need more money for integration and training. They also need to keep improving to stay safe and trusted.
Ethical Considerations in AI Healthcare Use
AI tools change how we work in healthcare and do research. But, we must think about the ethics of using them. We need good rules, clear who is in charge, and safety steps to use AI right.
Rules control how we share and use patient data. Laws like HIPAA in the U.S. and new rules in Europe help. We must make patient data safe for AI by removing personal info and checking it’s okay to use.
Getting data ready for AI is hard and expensive. We use special ways to keep data safe. This helps protect patient info and stops misuse.
AI must be fair. If the data used to train AI is not balanced, it can lead to unfair results. This can make some groups get worse care than others.
How we design AI matters. We should make AI explain its decisions clearly. This lets doctors understand what the AI is saying. Also, having humans check AI’s work helps catch mistakes before they harm patients.
Trust in AI grows when it works well in real life. We start with simple tasks and keep checking how it does. Having backup plans and alerts keeps things safe if AI goes wrong.
AI must fit how doctors work. If it doesn’t, it can cause problems. Making AI easy to use and part of the doctor’s routine helps everyone get along better.
Keeping AI ethical means always checking and making sure data is fair. A team with doctors, patients, ethicists, and tech experts should review AI. They check for bias and decide when to update AI.
Here’s a simple guide to how to manage AI in healthcare:
| Governance Element | Primary Benefit | Implementation Consideration |
|---|---|---|
| Data De-identification | Protects patient privacy AI and reduces legal exposure | Use k-anonymity, differential privacy; validate against re-identification attacks |
| Bias Audits | Improves equity and highlights disparities | Run subgroup performance tests; include demographically diverse datasets |
| Interpretability Tools | Builds clinician trust and enables oversight | Provide feature importance, probability scores, and case-level explanations |
| Human-in-the-Loop | Prevents automated errors from reaching patients | Define escalation paths and clear roles for clinicians |
| Continuous Monitoring | Detects model drift and safety issues early | Track performance metrics, log interventions, schedule audits |
| Inclusive Data Curation | Reduces bias and fairness in AI impacts | Engage community partners and acquire representative samples |
| Regulatory Compliance | Ensures legal alignment and patient protection | Map local laws, document data lineage, maintain consent records |
Using AI in healthcare is a team effort. It combines tech, medical knowledge, and rules to keep patients safe and help them get better care.
Future Trends in AI for Healthcare
The next decade will change how we work in healthcare. Places like Mayo Clinic and startups like Tempus are planning big changes. They want to mix clinical work with advanced analytics.
Advancements in machine learning
New models will soon be part of our daily work. Radiology and pathology will use these models to spot urgent cases quickly.
Cloud and edge compute will help doctors make decisions fast. This means less waiting and better care at the bedside.
Standard data formats will help train models better. This will make it easier to share data and improve algorithms.
AI and personalized medicine
AI will connect many things to make treatment better for each patient. This includes genes, health records, wearables, and images.
Clinical tools will give doctors real-time advice. They will get evidence and suggestions for each patient during visits.
Robots will help with everyday tasks. They will bring meds and restock, freeing up nurses for more important work. Surgery will also get better with AI, leading to better results and faster recovery.
Research and clear rules are key for AI in healthcare. Money is a big issue, so providers will start small. They will focus on getting ready for AI and learning to use it well.
AI and personalized medicine will make healthcare better. It will be more predictive, tailored, and efficient. But, we need to work together and make sure data works well.
Challenges Facing AI Implementations
AI could greatly improve healthcare, but it’s hard to put into practice. Leaders face many challenges like technical issues, legal hurdles, and getting people to use it. This article will explain the main problems and how to overcome them.
Integration with Existing Systems
Hospitals find it tough to make AI work with their current systems. These systems don’t always share data in the same way. This makes it expensive to get and organize the data.
Getting data clean and ready for AI is a big job. Health systems with little money have to think hard about if it’s worth the effort. They need to see if they’ll get a good return on their investment.
AI tools need to fit into how doctors work to be useful. Problems with how easy they are to use can slow down adoption. This is seen in tests of virtual assistants and chat systems.
Regulatory and Compliance Issues
Rules about privacy and data use are big hurdles for AI. In the U.S., HIPAA is key. But, rules in other countries are changing, making things even more complicated.
Regulators want solid proof that AI is safe and works well. But, many AI models don’t have enough testing. This makes it hard to get approval and use them widely.
There are also worries about who is responsible when AI makes mistakes. Doctors want clear, easy-to-understand advice from AI. This helps everyone know who to blame if something goes wrong.
Money and people are big factors in using AI. Setting up the right systems, training staff, and getting data ready costs a lot. Hospitals focus on areas where they can see clear benefits.
Doctors are more likely to accept AI if it’s introduced slowly. Starting with simple tasks like scheduling and paperwork can help build trust. Then, they can move on to more complex tasks.
It’s important to be able to compare AI tools in a fair way. For more details on how leaders view AI, check out this study: leader perspectives on AI implementation.
There are also big ethical concerns with AI. People worry about fairness, transparency, and who gets to use it. For more on these issues, see this article: challenges and ethics in medical AI.
- Action step: Focus on making AI work better with current systems.
- Action step: Start with small, easy tasks to build trust.
- Action step: Work on rules and clear lines of responsibility.
Conclusion: The Future of AI in Patient Care
AI in healthcare is real and helps a lot. It makes doctors’ work easier, helps find diseases faster, and speeds up finding new medicines. But, we need more data and better ways to use it.
Studies show AI is making healthcare safer and better. But, we need to make sure it works well everywhere. This means we need to test it more and make it clear how it works.
Call to Action for Healthcare Professionals
Doctors and leaders should focus on using data wisely. Start with small tests like making EHRs easier to read and automating schedules. It’s important to involve doctors in making these tools.
Also, we need to make sure these tools work well and are easy to use. Entrepreneurs should work with hospitals and schools to test their tools. This helps make sure they work for everyone.
Long-Term Vision for AI in Healthcare
In the next ten years, AI will help doctors a lot. It will make patient summaries and help find diseases quickly. Robots and remote systems will do routine tasks, so doctors can focus on caring for patients.
AI in healthcare needs careful use and rules. We also need to keep working on getting data ready. This way, everyone in the US can benefit from AI.
By working together and using data wisely, we can make AI in healthcare better. See this review for more on how to do it right in the literature. Also, check out recent studies on how AI is helping.
FAQ
What is "AI in healthcare" and what technologies does it include?
AI in healthcare uses advanced tech like neural networks and machine learning. It also includes natural language processing and large language models. These tools help analyze health data to find patterns and make predictions.
Why is AI important for modern healthcare?
AI helps solve big problems in healthcare, like aging populations and rising costs. It makes healthcare more efficient and accurate. AI can also help doctors work less and focus more on patients.
How does AI improve diagnostic accuracy?
AI helps doctors spot problems in medical images and lab results. It looks for patterns and makes suggestions. This makes diagnosis faster and more accurate.
Can AI create personalized treatment plans?
Yes, AI can tailor treatments based on a patient’s genes and health history. It helps doctors choose the best treatment for each person. This approach can lead to better health outcomes.
What clinical applications of AI deliver the biggest near-term impact?
AI can help with tasks like summarizing medical records and predicting patient risks. It can also improve medication safety and help with remote monitoring. These tools save time and improve patient care.
How does AI support medical imaging and image analysis?
AI helps doctors analyze medical images by highlighting important areas. It can also help with image triage and focus on complex cases. This makes diagnosis faster and more accurate.
Can AI reduce human error in clinical settings?
Yes, AI can help reduce mistakes by automating tasks and detecting anomalies. Studies show AI can lower certain types of errors. But, it needs good data and human oversight.
How does AI accelerate drug discovery and development?
AI can quickly screen drugs and predict their safety and effectiveness. It helps identify the most promising candidates. This saves time and reduces the risk of costly failures.
Is AI cost-effective for research and development?
AI can be cost-effective by focusing on promising leads and predicting safety issues. It helps make decisions faster. Early investments in data and validation can lead to big savings.
How do AI-driven virtual health assistants and remote monitoring systems work?
Virtual assistants help with tasks like scheduling and reminders. Remote monitoring uses sensors and AI to detect health issues early. These tools need careful design to avoid errors.
What are the primary privacy and data-security concerns with healthcare AI?
AI needs sensitive health data, which raises privacy concerns. Laws like HIPAA help protect data. Strong security measures and clear agreements are essential to keep data safe.
How does bias affect AI in healthcare and what mitigations exist?
AI can perpetuate biases if trained on biased data. To avoid this, use diverse data and transparent models. This helps ensure fair and accurate AI decisions.
What future trends will shape AI in healthcare?
Expect more advanced AI models and better integration with healthcare systems. Robotics and remote diagnostics will also become more common. These advancements will improve patient care.
How should healthcare organizations prioritize AI investments?
Start with small, high-value projects like EHR summarization. Focus on data quality and clinician involvement. Measure success to ensure AI benefits patients.
What integration and regulatory challenges do leaders face when deploying AI?
Integrating AI with existing systems is a big challenge. There are also regulatory hurdles to overcome. Leaders must plan for ongoing monitoring and compliance.
How can clinicians build trust in AI systems?
Trust comes from transparent validation and clear explanations. Start with low-risk uses and involve clinicians in design. Ongoing monitoring helps build confidence.
What operational benefits should health systems expect from AI adoption?
AI can save time on paperwork and improve patient flow. It helps detect risks early and reduce costs. Thoughtful AI adoption can lead to better operations.
Are there proven clinical outcomes from AI implementations?
Yes, AI has shown benefits in detecting errors and improving patient safety. Studies and reviews support its effectiveness. More real-world validation is needed.
What governance and quality practices are essential for safe AI use?
Ensure AI is validated on diverse data and monitored continuously. Use standardized reporting and data governance. This ensures AI is safe and effective.
How should entrepreneurs and innovators approach building healthcare AI products?
Focus on interoperability and clinician needs. Build partnerships with healthcare providers for real-world testing. Prioritize data quality and clear metrics to show value.
What is the long-term vision for AI in patient care?
AI will transform patient care over the next decade. It will help doctors focus on personalized care. Ethical use and data readiness will determine its success.