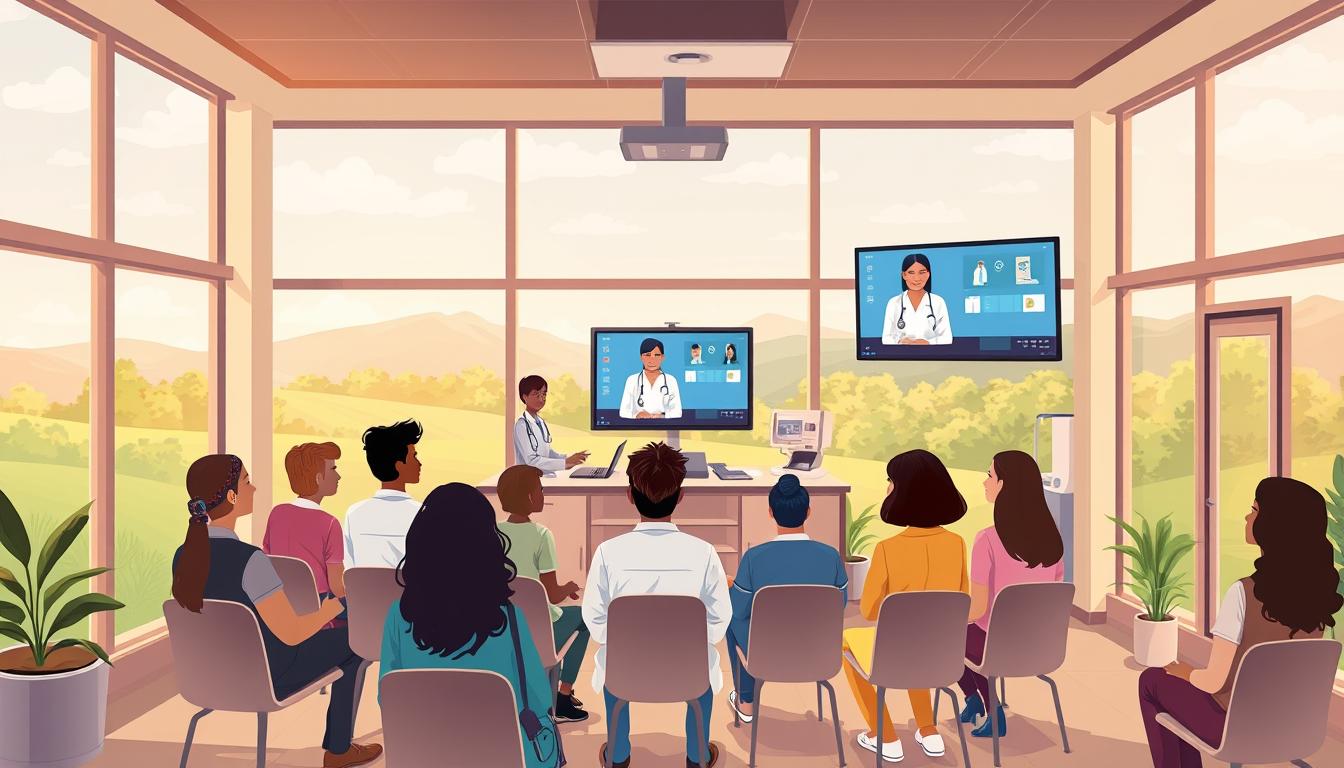
There are moments when a simple video call changes everything. A mother in rural Mississippi can talk to a pediatrician without a long trip. A working father in Phoenix can manage his health while keeping his job. A senior in Ohio gets care without leaving home.
This article shows how telemedicine helps everyone get fair care. More doctors use telemedicine now, thanks to COVID-19. Studies from 2010 to 2023 found many ways telemedicine can help.
Telemedicine is key to fair healthcare. It helps people who face big challenges. With the right design and policies, it can reach more people.
Key Takeaways
- Telemedicine offers measurable benefits of telemedicine for improving healthcare equity by expanding access across populations.
- Telehealth advantages include higher clinician adoption and sustained patient interest.
- Virtual care benefits are strongest where design and policy align with equity goals.
- Remote healthcare equality requires attention to affordability, awareness, and cultural fit.
- Implementing telemedicine strategically can reduce costs and improve outcomes at scale.
Understanding Telemedicine and Healthcare Equity
Telemedicine has grown from simple phone calls to big digital platforms. These platforms connect patients and doctors from far away. This section helps readers understand telemedicine through an equity lens.
Defining Telemedicine
Telemedicine includes many types of care, like video calls and sending health info online. It also includes tracking health remotely and looking at medical images from afar. These services need fast internet, devices, and doctors’ time.
Digital health technology (DHT) is about using computers and software for health care. It can work in many languages and places. This makes it better for people when it’s designed with them in mind.
What is Healthcare Equity?
Healthcare equity means everyone gets the same care, no matter who they are. The World Health Organization says it’s about everyone being as healthy as they can be.
Things like where you live, how much you make, and your education affect your health. To make things fair, we need to work on policies and programs at all levels.
- Design must address algorithmic bias and the digital divide; it risks making things worse.
- We should check six things: how easy it is to get care, if it’s there, if it’s okay, if it’s affordable, if it’s enough, and if people know about it.
- Having clear plans and looking at many angles helps make telemedicine work better.
Telemedicine can help make healthcare fairer if we make smart choices. We need to design products that include everyone, make sure everyone can use them, train doctors, and improve internet and devices. When we do, telemedicine can help more people get the care they need.
How Telemedicine Bridges Healthcare Gaps
Telemedicine changes where and how we get care. It removes distance as a big problem. This makes it easier for everyone to get healthcare.
Expanding Access for Rural Communities
People in rural areas often have to travel far to see doctors. Telemedicine lets them talk to doctors from home. This makes it easier to get care and keeps appointments.
But, not everyone in rural areas can use telemedicine because of internet issues. During the COVID-19 pandemic, rules changed to help. Keeping these rules helps more people get care.
To make telemedicine work, we need better internet, training, and ways to mix online and in-person care. When we do this, more people can get care at home or in clinics.
Connecting Underserved Populations
Digital health tools can be made for different languages and cultures. This helps low-income and minority groups. It makes it easier for them to get care.
But, we need more research and better ways to pay for telemedicine. Programs that help with devices and internet costs work better. They make sure everyone can get care.
A study found 82 ways to make telemedicine better. It suggests using telemedicine with community help and money. This way, we can make sure everyone gets the care they need.
Improved Accessibility for Vulnerable Groups
Virtual care helps those who can’t easily get to doctors. It’s good for people with mobility, sensory, or transport issues. But, how well it works depends on design and policy.
Enhancing Care for the Elderly
Telemedicine means less travel for older adults. It’s safer for them, too. They can get care at home, without going to the clinic.
It’s important for seniors to use it easily. Simple designs and quick training help. Places like Kaiser Permanente and Cleveland Clinic are making it better for seniors.
Supporting Patients with Disabilities
Remote visits help those who can’t get to clinics easily. They make communication better for people with hearing, vision, or cognitive issues. This is thanks to features like captioning and screen-reader compatibility.
Some tests need to be done in person. But, telemedicine can handle routine care. This way, everyone gets the care they need.
Accessibility and affordability are key. Platforms must be ADA-compliant and offer interpreter services. This way, everyone can use virtual care and get better healthcare.
Cost Effectiveness of Telemedicine
Telemedicine helps lower healthcare costs. It saves money on direct and indirect costs. It also helps reduce healthcare disparities.
Stakeholders need to look at both sides. They should see the savings from fewer missed appointments. They should also consider the costs of equipment and broadband.
A balanced view is key. It helps policymakers and providers create sustainable programs. These programs should make care more accessible without passing hidden costs to patients.
Reducing Travel Expenses
Remote visits save patients money on travel. They save on transportation and parking. This is big for those in rural areas who have to travel far.
Less travel also means fewer no-shows. This frees up clinic space for more urgent care.
Studies on cost outcomes are mixed. A review found some studies showed telemedicine saves money. But, it also pointed out some studies were not of high quality. One analysis found some studies said telemedicine is cost-effective.
Minimizing Lost Income
Telehealth lets working adults and caregivers stay at work. This saves them money on lost wages and childcare. It’s a big help for low-income families.
Payment policies affect how affordable telehealth is. Before the pandemic, Medicare paid less for telehealth. The pandemic changed this, making telehealth more appealing. But, if these changes are not permanent, telehealth might not stay affordable.
Programs need to think about data plans and device upkeep. They should also consider technical support. Making sure reimbursement is fair and providing low-cost devices can make telehealth more appealing. Expanding broadband is also important for reducing healthcare disparities.
Convenience and Flexibility in Healthcare
Telemedicine changes how we get care. It offers more times to see doctors, shorter visits, and check-ins from home. This makes it easier for people with busy lives.
Overcoming Scheduling Conflicts
Virtual appointments mean care at any time. They fit into busy days. This helps workers, parents, and those with limited travel options.
Clinics need to work well to use telehealth fully. Without good planning, it’s hard to get appointments.
Fostering Consistent Follow-Up Care
Remote monitoring helps with chronic conditions like diabetes. It lets doctors catch problems early. This means better care for patients.
Regular check-ups help avoid broken care. When clinics work together, patients get better care. This leads to fewer emergency visits.
To make care better, clinics can change their schedules. They should also train staff for telehealth. This makes quality care available to everyone.
Enhanced Patient Engagement and Satisfaction
Telemedicine makes care more personal by being quicker and more flexible. This helps make healthcare better for everyone. It shows how telehealth can really help patients.

Now, we have tools like secure messaging and video visits. These help doctors meet what patients want. When these tools are easy to use and in many languages, more people are happy.
Utilizing technology for better communication
Tools like remote monitoring help keep up with patients. Patients feel closer to their doctors when care is tailored. How easy something is to use matters a lot.
Encouraging patient-centered care
Telemedicine makes it easier to involve patients in decisions. It’s great for those who need flexible schedules. This way, care is more about what patients need.
But, there are worries about trust. Things like biased tech and not knowing how to use it can be a problem. Being open about how tech works helps fix these issues.
Teams can make a difference by focusing on people and being clear about data. This way, telemedicine can really help make healthcare fairer. It shows how telehealth can make a big difference in care.
| Focus Area | Action | Expected Effect |
|---|---|---|
| Communication tools | Offer secure messaging, video, and remote monitoring | Faster responses, improved adherence, higher satisfaction |
| Cultural and language adaptation | Localize interfaces and provide interpreter support | Greater trust, higher uptake among diverse groups |
| AI transparency | Publish model use and bias mitigation steps | Increased trust, reduced disparities |
| Digital literacy | Provide simple tutorials and live support | Broader access and sustained engagement |
Addressing Language and Cultural Barriers
Virtual care can help patients who face language or cultural obstacles. Health systems can make telemedicine solutions better by adding interpreter access and cultural adaptation. Small changes, like translated menus and patient education, can make a big difference.
Telehealth platforms offer more flexible video and audio interpreting than in-person settings. This flexibility helps doctors connect with patients who don’t speak English well. Steps like scheduling interpreters ahead and training staff are important.
Telehealth and Interpreter Services
Adding professional interpreters needs planning. This includes setting up interpreter requests and checking if they understand correctly. Places like Kaiser Permanente and Cleveland Clinic have shown how to do this well.
Many reviews talk about access issues, but opinions vary. A review found that many studies said it was okay to use telehealth. You can read more about it here: acceptability in telehealth reviews.
Embracing Diverse Cultural Needs
Digital health tools can be made to fit different cultures. Adding language variants and culturally relevant examples helps. This makes treatment more effective.
It’s important to involve the community. Working with local leaders and patient advocates helps. Some people prefer in-person visits, while others like virtual care. Building trust through outreach can help.
| Focus Area | Practical Action | Expected Impact |
|---|---|---|
| Interpreter Integration | Embed three-way calling, schedule interpreters, certify vendors | Improved communication, fewer misunderstandings |
| Localization | Translate UI, adapt education materials, test readability | Higher engagement, better adherence |
| Community Co-design | Host focus groups, partner with faith and civic leaders | Greater trust, tailored solutions accepted |
| Measurement | Track use of interpreters, survey cultural acceptability | Actionable insights to refine telemedicine solutions |
Designers and leaders should make cultural adaptation a priority. This makes telehealth better for everyone and helps those who were left behind.
Regulatory Changes Supporting Telemedicine
Policy changes in 2020 changed how doctors care for patients. Medicare and private payers relaxed rules to let care happen at home. This move helped more people get care without leaving their homes.
Recent Legislative Advances
New laws want to make these changes permanent. The CONNECT for Health Act wants to keep more telehealth options. The American Medical Association supports these changes to keep care accessible.
Studies show these changes help a lot. They help with chronic diseases and make patients happier. They also cut down on travel. You can learn more about this in a study.
State Licensure and Telehealth Parity
States are making it easier for doctors to work across borders. This helps doctors reach more people in rural areas. It makes telemedicine better for everyone.
But, payment for telemedicine is not always fair. Some places pay the same for online visits as in-person ones. But others don’t. It’s important to make sure doctors get paid fairly for their work.
To keep telemedicine good, we need to fix a few things. We need better internet, rules for online prescriptions, and help for doctors in tough places. We also need to make sure everyone can get telemedicine, no matter where they are.
The Future of Telemedicine in Promoting Equity
Telemedicine is getting smarter and more inclusive. New tech like generative AI will help talk to people in their own way. It will also help manage diseases better.
These changes will make healthcare better for everyone. They will help those who need it most.
Innovations on the Horizon
New tools will help reach more people. They will talk in many languages and use health data from wearables. But, we must be careful with AI to avoid mistakes.
We need to make sure AI is fair and safe. This means using good data and listening to communities.
Long-Term Impact on Healthcare Systems
Telemedicine can make healthcare better for all. It can be more affordable and accessible. But, we need to make sure it works for everyone.
We need to invest in the right things. This includes good internet, devices, and training. A report has a plan to make this happen here.
To really make a difference, we need everyone to work together. We must invest in the right things and make sure it’s fair. Telemedicine can be a big help if we do it right.
FAQ
What is telemedicine and which modalities does it include?
Telemedicine, also called telehealth, includes many ways to care for patients remotely. This includes video calls, messaging, and monitoring health from afar. It needs special devices, internet, and rules to work well.
How is healthcare equity defined in this context?
Healthcare equity means everyone gets the care they need without unfair differences. It’s about making sure everyone can be as healthy as they can be. This means fixing problems like lack of food or safe homes.
How does telemedicine expand access for rural communities?
Telemedicine helps people in rural areas get care without traveling far. During the COVID-19 pandemic, it became even easier to get care at home. Keeping these options open is key.
Can telemedicine effectively connect underserved urban and low-income populations?
Yes, if it’s made with fairness in mind. It can make getting care easier and more personal. But, it needs to be affordable and easy to use for everyone.
How does telemedicine improve care for older adults?
It helps older adults get care without leaving their homes. This is good for their health and safety. It works best if devices are easy to use and caregivers help.
In what ways does telehealth benefit patients with disabilities?
It helps patients with disabilities by making visits easier to get to. It also works with tools that help them communicate better. Care needs to be designed for their needs.
Does telemedicine reduce patient costs like travel and lost wages?
Yes, it can save money by cutting down on travel and lost work time. This is a big help for those who can’t afford to lose money. But, it depends on how it’s paid for.
How does telehealth help overcome scheduling conflicts?
It offers more flexible times for visits, like after work or on weekends. This helps people who can’t get to the doctor during regular hours. But, doctors need to be available too.
Can telemedicine improve continuity and follow-up care?
Yes, it helps keep track of health over time. This is good for managing chronic conditions and catching problems early. It works best if doctors can follow up regularly.
How do digital tools enhance patient communication and engagement?
Tools like messaging and monitoring help patients stay in touch with their care team. Making these tools easy to use and understand helps more people use them. It’s also important to be open about how they work.
What role do interpreter services play in telehealth?
Interpreter services help patients who don’t speak the same language as their doctor. This is done through video or phone calls. It’s important to make sure interpreters are part of the care plan.
How can telemedicine be adapted to diverse cultural needs?
Digital health tools can be changed to fit different cultures and languages. It’s important to work with communities to make sure they are useful and accepted.
What recent policy changes have supported telemedicine expansion?
During the COVID-19 pandemic, rules were relaxed to make telemedicine easier. This helped a lot of people get care without leaving home. Now, there are efforts to keep these changes in place.
How do state licensure and parity laws affect telehealth equity?
Laws that let doctors work across states help more people get care. Laws that make sure telehealth is paid for the same as in-person care also help. But, different states have different rules, which can make things uneven.
What innovations in telemedicine could further advance equity?
New technologies like AI can make care more personal and accessible. Tools that help monitor health and combine different types of care can also help. But, these need to be fair and tested on different groups.
What is the likely long-term impact of telemedicine on healthcare systems and disparities?
Telemedicine could make healthcare better and more fair over time. It can help more people get care, save money, and keep health on track. But, it needs fair rules and support to really help those who need it most.